Abstract
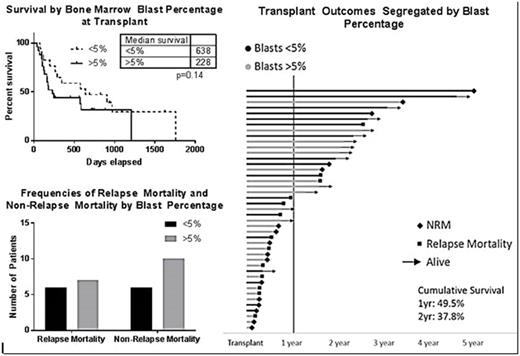
For patients with acute myeloid leukemia (AML) who fail to achieve complete remission (CR) after induction chemotherapy, allogeneic stem cell transplantation (Allo-SCT) can provide leukemia control and result in long-term survival (Blood. 2016;127(1):53-61; BBMT. 2003;9(12):766-71; BBMT. 2016;22(10):1867-73). In this retrospective study, we analyzed the outcomes of patients at our institution who had chemotherapy-resistant AML and subsequently received Allo-SCT. We defined "chemotherapy-resistant AML" as not achieving CR prior to transplant according to the Center for International Blood & Marrow Transplant Research (CIBMTR) reporting criteria after one or more cycles of induction chemotherapy. We queried our CIBMTR reporting data and identified 44 patients age ≥ 18 years with AML who were not in CR and who were transplanted from 2009 to 2015. Patient records were reviewed and the following variables were collected: age, KPS, cytogenetic risk, number of prior chemotherapy cycles, chemotherapy regimens, transplant conditioning regimens, stem cell donor characteristics, blasts percentage at time of transplantation, and key transplant outcomes (overall survival, OS; relapse mortality; and, non-relapse mortality, NRM). Key transplant outcomes were segregated by blast percentage at time of transplantation (≤5% v. >5%) and analyzed. The median age was 60 years (range 20-73 years), and the median KPS was 62%(range 50-100%). Most patients received 2 or more induction regimens prior to transplant (n=32, 72%). Based on the MRC 2010 cytogenetic risk classification system (Blood. 2010 116:354-365), cytogenetic risk was classified as intermediate risk in 23 patients and unfavorable risk in 21 patients. Molecular markers and targeted gene sequencing were not available in most cases. Myeloablative conditioning was used in 29 patients (65%). Stem cell donors were as follows: matched related donor (n= 6; 13.9%), 10/10 or 9/10 matched unrelated donor (n=25, 56%), haploidentical donor (n= 6; 13.9%), and cord blood donor (n= 6; 13.9%). Stem cell sources were as follows: peripheral blood (n= 34; 79%), bone marrow (n= 3, 6.9%), and cord blood (n= 6; 13.9%). Blast count at the time of transplant ranged from <5% to as high as 55%; 18 patients (41%) had blast count >5% at the time of transplant. With a median follow up of 553days, cumulative 1-year and 2-year survival for the entire cohort was 49.5% and 37.8%, respectively. Most of the deaths occurred within the first year after the transplant (n=21; 49%). Of the 30 deaths, relapse preceded death in 17 patients (57%). A graphical representation of outcomes (swimmer plot) summarizes the post-transplant outcome for each of the 44 patients (Figure 1). Our data suggest that elevated blast percentage pre-transplant may impact survival outcomes in patients with chemotherapy-resistant AML, through the results were not statistically significant (Figure 1; ≤5% blasts median OS 638 days v. >5% 228 days; p=0.14). Approximately equal numbers of patients died from disease relapse and NRM in this high-risk cohort regardless of the blast percentage prior to transplantation (Figure 1). A third of patients are currently alive and disease free (n=14; 32%), with relatively equal numbers in the ≤5% blast and >5% blast groups (n=8 v. n=6). Although our study involves a small population of patients, we conclude that the approach to this high-risk subgroup of patients requires further study and a more standardized approach. Strategies to reduce non-relapse mortality (improved conditioning regimens) and relapse mortality (post-transplant maintenance strategies) are equally important in this group who otherwise have few treatment options.
Lin: Jazz Pharmaceuticals: Consultancy. Ganguly: Amgen: Other: Advisory Board; Seattle Genetics: Speakers Bureau. Skikne: Celgene Corporation: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal